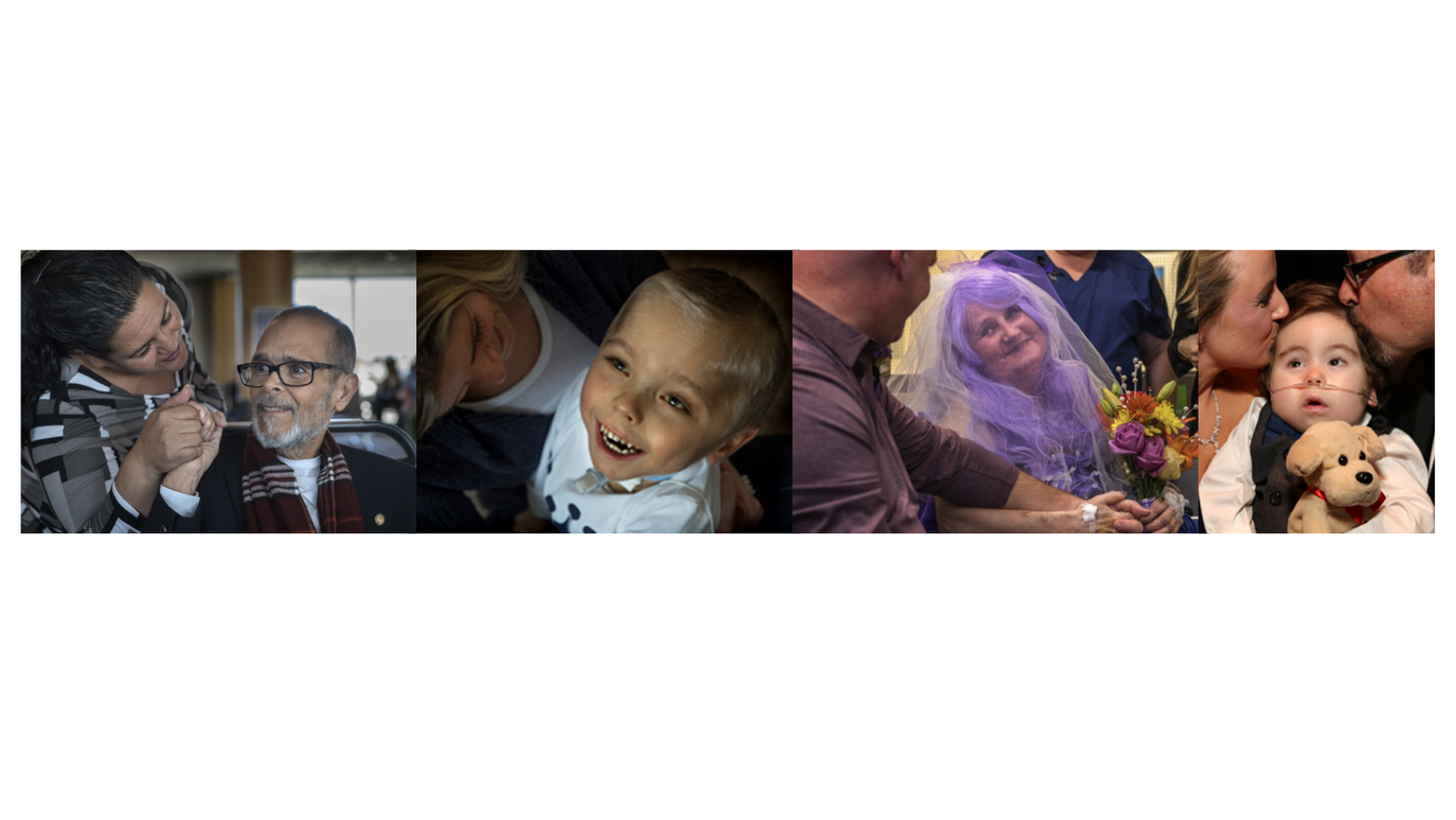
Hospice and palliative medicine fellowship


The Corewell Health – Grand Rapids/Michigan State University Hospice and Palliative Medicine Fellowship is an ACGME-accredited one-year program located in Grand Rapids, Michigan. Established in 2021, our fellowship offers both an adult and pediatric track. Our main training sites are Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals), a 556-bed, level 1 trauma center and Corewell Health Helen DeVos Children's Hospital (part of Corewell Health Grand Rapids Hospitals), a 234-bed regional referral center and teaching hospital and is located on the same campus as Butterworth Hospital.
From the Program Director
Thank you for your interest in the Corewell Health – Grand Rapids/Michigan State University Hospice and Palliative Medicine Fellowship! Our mission is to provide exceptional training focused on interdisciplinary, patient-directed care across the health care continuum. Upon completion of training, fellows will have the experience and training to work in any environment within the field of hospice and palliative medicine.

Fellowship Retreat at Camp Geneva
This program focuses on practicing evidence-based medicine, seeking innovative solutions to optimize patient care, understanding the impact of health disparities and the complex relationship with social determinants, and continual quality improvement. We view medical care through the lens of equity and this is reflected in all that we do. Working in urban and community environments, fellows in our program will serve patients in alignment with our institution’s mission of improving health, inspiring hope and saving lives. This includes the quality of lives.
Our adult and pediatric teams provide a comprehensive educational experience. Working with high functioning interdisciplinary teams, fellows will have exposure to a variety of advanced and serious illnesses and will develop skills in complex symptom management and communication and goals of care discussions. Our interdisciplinary teams include physicians, advanced practice providers, nurses, social workers and chaplains. Throughout Corewell Health in West Michigan, we have an integrated and respected inpatient palliative care service, ambulatory and virtual palliative clinics, community palliative care service, as well as inpatient and community hospice teams who provide seamless care for our patients. Fellows will follow patients across the continuum of care which enhances their learning experience and continuity with patients and families.
You will find an engaging and supportive environment in this fellowship program as we strive to provide exceptional, compassionate care to our patients in addition to focusing on team and individual wellness, resiliency and self-care. We accept applicants from diverse backgrounds and specialties and encourage applicants from all phases of their career. We hope to personalize your training, provide mentorship and career-development based on your goals and passions.
We can assure you that upon completion of this fellowship you will feel well trained for any career in the field of hospice and palliative care. We hope you find this information useful in your decision-making process. Thank you for considering us for your fellowship training and please reach out with any questions.
Gretchen Roe, MD
Program Director, Hospice and Palliative Medicine Fellowship
Assistant Professor, Michigan State University
gretchen.roe@corewellhealth.org
Bradd Hemker, MD
Associate Program Director, Hospice and Palliative Medicine Fellowship (Pediatric Track)
Division Chief, Comprehensive Care
Section Chief, Pediatric Pain and Palliative Medicine
Clinical Assistant Professor, Michigan State University College of Human Medicine
bradd.hemker@helendevoschildrens.org
Program Highlights
- Program aims
- Integrated and respected inpatient palliative care service, ambulatory palliative clinics with options for telemedicine and virtual visits, community palliative care service, as well as an inpatient and community hospice team
- Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals) is a referral center for advanced cardiac therapies including extracorporeal membrane oxygenation and left ventricular assist devices (LVADs), and transplant center for heart and lung transplants. Palliative care is involved as part of the pre-assessment for all heart and lung transplants and LVADs, playing an integral role on the LVAD selection committee
- Fellows will see a variety of medically complex and critically ill children at Corewell Health Helen DeVos Children's Hospital (part of Corewell Health Grand Rapids Hospitals)
- All hospice and palliative medicine faculty are board-certified and come from diverse backgrounds and specialties, including internal medicine, pediatrics, family medicine and emergency medicine and bring experiences from multiple health systems across the country
Corewell Health in West Michigan is home to 37 ACGME-accredited residency and fellowship programs in partnership with Michigan State University College of Human Medicine
- There are opportunities to partner with other fellowship programs within our institution including the fellowship research and QI didactic series
- Our affiliation with Michigan State University College of Human Medicine allows for a unique, hybrid community and academic practice environment
- Fellows have research support through Corewell Health and Michigan State University
Education
Clinical rotations: There are 13 blocks, each block being four weeks.
Adult Track
Inpatient palliative care: 5.5 blocks
Community Hospice: 2 blocks
Inpatient Hospice: 1.5 blocks
Home palliative: 1 block
Geriatrics (long-term care): 1 block
Pediatric Palliative Care: 1 block
Elective: 1 block
Pediatric Track
Pediatric Palliative Care: 6 blocks
Inpatient palliative care: 1.5 blocks
Community Hospice: 2 blocks
Inpatient Hospice: 1.5 blocks
Geriatrics (long-term care): 1 block
Elective: 1 block
Inpatient palliative care
This rotation will mainly be at Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals), a 556-bed, level 1 trauma center, referral center for advanced cardiac therapies including extracorporeal membrane oxygenation and left ventricular assist devices (LVADs), and transplant center for heart and lung transplants. Palliative care is involved as part of the pre-assessment for all heart and lung transplants and LVADs, playing an integral role on the LVAD selection committee. There is a robust oncology inpatient service including a bone marrow transplant service. Fellows will experience collaboration with the interventional radiology and anesthesia services regarding procedures to minimize suffering and optimize quality of life. The experience will include working with interdisciplinary palliative and hospice teams and collaboration with multiple specialties, participating in goals of care discussions and complex symptom management. We incorporate one week of addiction medicine experience during inpatient palliative care months. Fellows will also have the opportunity to care for patients at Corewell Health Blodgett Hospital (part of Corewell Health Grand Rapids Hospitals) during their inpatient rotations. Located in East Grand Rapids, it provides inpatient care in 248 private patient rooms and outpatient services for medical, surgical and specialty care.
Community hospice
In their community hospice experience, fellows will work with the interdisciplinary hospice team and participate with goals of care discussions and symptom management during home visits as well as perform face-to-face visits. They will learn the role of a hospice medical director, hospice regulations, hospice eligibility, and actively participate in interdisciplinary groups and learn how to write hospice certification and re-certification notes.
Inpatient hospice
The inpatient hospice experience includes collaborating with an inpatient interdisciplinary hospice team, participating in goals of care discussions and symptom management for general inpatient hospice patients including symptom management after withdrawal from LVAD and other advanced cardiac therapy support as well as withdrawal from mechanical ventilation, BIPAP, and high flow nasal cannula. Fellows will assess hospice eligibility for new hospice referrals for inpatients. In addition to this experience in the hospital setting, fellows will round in the supportive care unit which is our six-bed inpatient hospice unit located within a local nursing facility.
Home-based palliative care
Fellows are part of the interdisciplinary team visiting patients in their homes and skilled nursing facilities. Participation in goals of care discussions, thorough home environment assessments, establishing symptom management plans, recognizing safety components for both staff and patient/family, exploring outside community resources, support to families and collaboration with various providers are essential functions in this rotation. Throughout the 11-county service territory, fellows will learn the physician role in this ever-changing program and the unique challenges and opportunities that being out in the community brings. Ability to participate and lead Interdisciplinary Group meetings, break down barriers to hospice transitions, deep dive into social determinants of health, brainstorm creative support needs and communicate efficiently with internal and external partners will be the focus of expanding knowledge of palliative care services in this track.
Geriatrics
Under supervision of a geriatrics attending physician, fellows will evaluate patients then discuss findings to gain greater understanding of geriatric syndromes including delirium, cognitive impairment and dementia, gait disorders and falls and polypharmacy. This rotation emphasizes transitions in care and understanding different health care settings as microsystems. Focusing on the older adult population that displays significant heterogeneity of health status, the rotation will make it possible to learn how to distinguish frail from healthy older adults and their differing levels of vulnerability. Fellows will also understand how care for older adults evolves from an intent that is curative to a strictly palliative intent for patients who may transition from independent living at home or a life care community, to hospital, home with home care, subacute rehabilitation or long-term care and eventually hospice. Fellows will also spend time at Butterworth Hospital with the Geriatric Trauma Service.
Pediatric hospice and palliative medicine
Fellows participate in daily rounds with the interdisciplinary pediatric palliative care team caring for children at Helen DeVos Children’s Hospital. Fellows will see a variety of medically complex and critically ill children in multiple settings, including the neonatal intensive care unit, pediatric intensive care unit, pediatric cardiac intensive care unit, inpatient oncology unit and the general pediatric units. Fellows will participate in pre-natal consults with expectant mothers whose children have severe anomalies diagnosed in-utero. They will also follow patients in a dedicated ambulatory palliative care clinic and provide home visits when appropriate. They will provide end-of-life care for children admitted to the hospital from hospice when inpatient services are required. Fellows will spend time with a dedicated pediatric team of a local community-based hospice to gain experience with home hospice care of pediatric patients.
Elective
Many elective experiences are available to fellows and the experience will be tailored to their goals and objectives. Options include, though are not limited to, clinical ethics, leadership and administration, medical education, addiction medicine, child life, anesthesia and pain service and interventional radiology.
Ambulatory clinics
Fellows will have a weekly half-day continuity clinic throughout fellowship. During the majority of blocks, this will occur in the adult palliative oncology clinic at Corewell Health Lemmen-Holten Cancer Pavilion. There will also be opportunities for spending time in the palliative advanced heart failure clinic and lung transplant clinic during the community hospice and palliative care rotation and geriatrics clinic during the geriatric rotation. Pediatric fellows will have additional pediatric pain and palliative clinic experience built into their pediatric rotations. Each of these clinics has an interdisciplinary approach.
Didactics
- Weekly didactics with interactive lectures in partnership with regional HPM programs.
- Serious Illness Communication Course
- Fellows receive training in mastering tough conversations through longitudinal sim sessions
- Our year-long curriculum is based on Vital Talk - an industry leading, evidence-based, serious illness communication course
- Simulation sessions are facilitated by Vital Talk accredited faculty and professional standardized patients
- Monthly journal club
- Monthly Schwartz Rounds
- Protected time to attend the annual assembly of the American Academy of Hospice and Palliative Medicine
- Fellows Research Education Series
- Clinical Teacher Program
- Quality and Safety curriculum
- Case presentations during daily team huddles with teaching from a diverse group of practitioners with a large depth and diversity of experience
- Fellows have the opportunity to teach resident and medical student rotations with our hospice and palliative teams
- Billing/Coding/Documentation training
- Robust Diversity, Equity and Inclusion curriculum (including participation in the Hospice & Palliative Medicine DEI committee)
- Palliative Complex Pain Panel (interdisciplinary discussion of patients with complex pain)
Scholarly activity
Fellows have protected time to complete a scholarly activity during their fellowship and will be provided mentorship for their scholarly activity by our faculty. Examples of options for scholarly activity include presenting at a local or regional conference, submission of a case report or other article, or a quality improvement project. Corewell Health in West Michigan provides many opportunities in clinical, quality and safety-based research. Corewell Health and Michigan State University have a growing interest in multi-center collaborative research networks.
Application requirements
We participate in the Electronic Residency Application Service application process. We require the following information:
- A completed application/profile
- At least three letters of recommendation
- Curriculum vitae
- Medical school transcript and dean’s letter
- Personal statement describing career goals and reasons for selecting continued training
- USMLE transcript
- For international medical graduates, an Educational Commission for Foreign Medical Graduates status report
For more information on our program, contact Jennifer Bruno, program coordinator.
Salary and benefits
Corewell Health in West Michigan provides a comprehensive and very competitive benefits package for our residents, staff and their families. In addition, our program provides educational monies to support your ongoing education. Download our salary and benefits document to learn more.
Explore West Michigan


Food: Release your inner foodie exploring one of the top food cities in the US.
Entertainment: From zoos and museums to festivals and art, there is a new experience around every corner.
Shopping: West Michigan has a diverse assortment of shops for everyone.

Outdoors: With trails, lakes and more, there is so much of West Michigan to explore.
Sustainability: Located along the shore of Lake Michigan, West Michigan has many initiatives to protect our natural resources.

Identities matter and so do you! Our residency and fellowship programs offer social activities, wellness programs and a diversity council to foster respect, personal health and community.
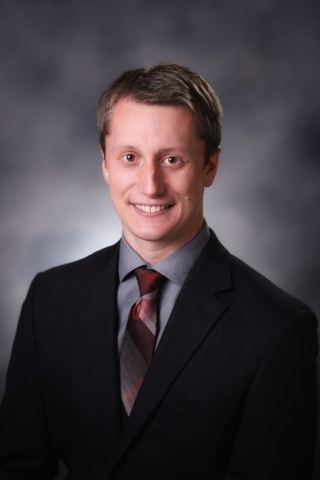
Program Director

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Emergency Medicine
- Fellowship: Grand Rapids Medical Education Partners
- Residency: Carolinas Medical Center

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Emergency Medicine
- Fellowship: Grand Rapids Medical Education Partners
- Residency: Carolinas Medical Center
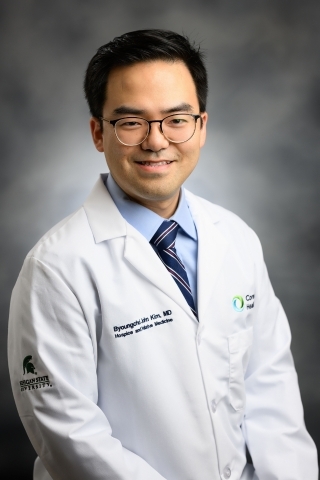
Associate Program Director

Pediatric Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Pediatric Hematology-Oncology
- Fellowship: Children's Hospital of Boston
- Medical College of Wisconsin
- Residency: Loyola University of Chicago

Pediatric Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Pediatric Hematology-Oncology
- Fellowship: Children's Hospital of Boston
- Medical College of Wisconsin
- Residency: Loyola University of Chicago
Core Faculty

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Emergency Medicine
- Fellowship: Henry Ford Health System
- Residency: University of Michigan

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Internal Medicine
- Residency: Michigan State University

Pediatric Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Pediatrics
- Fellowship: Grand Rapids Medical Education Partners
- Residency: Grand Rapids Medical Education Partners
Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Family Medicine
- Fellowship: Spectrum Health/Michigan State University
- Residency: Spectrum Health/Michigan State University

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Emergency Medicine
- Fellowship: Henry Ford Health System
- Residency: University of Michigan

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Internal Medicine
- Residency: Michigan State University

Pediatric Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Pediatrics
- Fellowship: Grand Rapids Medical Education Partners
- Residency: Grand Rapids Medical Education Partners
Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Family Medicine
- Fellowship: Spectrum Health/Michigan State University
- Residency: Spectrum Health/Michigan State University

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Family Medicine
- Fellowship: Mercy Health - Grand Rapids
- Residency: Mercy Health - Grand Rapids

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Internal Medicine
- Fellowship: University of Michigan
- Residency: Grand Rapids Medical Education Partners

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Family Medicine
- Residency: Grand Rapids Medical Education Partners

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Family Medicine
- Fellowship: Trinity Health Grand Rapids (formerly Mercy Health)
- Residency: University of Michigan Health West (formerly Metro Health)

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Family Medicine
- Residency: University of Michigan

Hospice and Palliative Care Physician
- Specialty: Hospice and Palliative Medicine; Internal Medicine
- Fellowship: University of Minnesota
- Residency: University of Michigan

Geriatrician
- Specialty: Geriatrics; Family Medicine
- Fellowship: Johns Hopkins University
- Residency: University of Michigan

Hospice and Palliative Care Specialist

Hospice and Palliative Care Specialist

Hospice and Palliative Care Specialist

Hospice and Palliative Care Specialist
PGY 4

Pediatrics: Children’s Hospital of Michigan

Emergency Medicine: Detroit Medical Center
*Adult Track
Internal Medicine: Trinity Health Grand Rapids
*Adult Track

Pediatrics: Children’s Hospital of Michigan

Emergency Medicine: Detroit Medical Center
*Adult Track
Internal Medicine: Trinity Health Grand Rapids
*Adult Track
Ready to Apply?
We participate in the National Resident Matching Program and use the Electronic Residency Application Service.
